Cardiac toxicity is damage to the heart by harmful chemicals. You may be given toxins (drugs) to kill cancer cells as part of your treatment. A side effect is that the normal cells in and around your heart can also be killed. Besides cell death, other types of cardiac toxicity from cancer treatment include:
Cardiomyopathy is when the heart muscle becomes weakened, enlarged, thickened, or stiff. This can lead to changes in heart rhythm or heart failure.
Myocarditis is inflammation (swelling) of the heart. This can lead to changes in heart rhythm or heart failure.
Pericarditis is inflammation (swelling) of the sac surrounding the heart. This can cause chest pain or heart failure.
Acute coronary syndromes are caused by blood vessel damage, which reduces blood flow to the heart. This can cause chest pain or a heart attack (myocardial infarction).
Congestive heart failure is when the heart cannot pump enough blood throughout the body. Chemotherapy can cause mild or severe damage to the heart. If severe, congestive heart failure or other life-threatening problems can occur. A heart transplant may even be needed.
What cancer treatments cause cardiac toxicity?
Chemotherapy
The chemotherapy drugs that most commonly cause heart damage are anthracyclines. Anthracyclines are used to treat many types of cancers. Examples include some types of leukemia, lymphoma, and sarcomas, as well as bladder, bone, breast, head and neck, kidney, skin, stomach, and other cancers. Anthracyclines include:
Daunorubicin (Cerubidine®),
Doxorubicin,
Doxorubicin liposome injection (Doxil®),
Epirubicin (Ellence®),
Idarubicin (Idamycin® PFS), and
Valrubicin (Valstar®)
In rare cases, cyclophosphamide can damage the heart. This chemotherapy drug is an alkylating agent. It is sometimes used to treat some types of leukemia, lymphoma, myeloma, and sarcomas, as well as bone, breast, central nervous system, ovarian, and skin cancers.
Targeted therapy
Targeted therapy drugs that can cause damage to the heart include trastuzumab (Herceptin®), bevacizumab (Avastin®), lapatinib (Tykerb®), sunitinib (Sutent®), and sorafenib (Nexavar®). These drugs are used in a variety of cancer types.
Radiation therapy
Many patients with cancer get radiation therapy to the chest. Examples of cancers that may be treated with radiation include breast, lung, lymphoma, and some childhood cancers. This radiation can damage the blood vessels that bring blood to the heart. Patients who are treated with both anthracyclines and radiation to the chest are at high risk for heart problems. So are patients who are treated with both anthracyclines and trastuzumab.
Who is at increased risk for cardiac toxicity?
Older patients, young children, and women risk cardiac toxicity more. In addition, patients with other health conditions at the same time as cancer is at increased risk. This is especially true for patients with signs of heart trouble before cancer.
What are the symptoms of cardiac toxicity?
Arrhythmias are health problems with the speed or rhythm of the heartbeat. You may not notice any symptoms. Then again, you might have chest pain or see changes in your heart rhythm. Atrial fibrillation is the most common type of arrhythmia. It is an abnormal beating of the heart’s upper left chamber. It is common not to notice atrial fibrillation.
Your doctor may tell you you have a decline in LVEF (left ventricular ejection fraction). This means your heart isn’t pumping as much blood with each heartbeat as it should. Your treatment will likely be changed if this happens, and you may be started on drugs to help your heart.
If the damage is severe, you may have congestive heart failure. You may feel exhausted and have trouble breathing. You will first notice the shortness of breath when you are active. Later, you will be short of breath even while resting. Congestive heart failure causes you to gain weight and your ankles to swell. You may also find it uncomfortable to lie on your back.
You might not notice these symptoms until many months or even years after you have completed cancer treatment. Tell your doctor if any of these symptoms start.
How is cardiac toxicity diagnosed?
Your heart will likely be checked before you start treatment. This will tell your doctor about your baseline (pre-treatment) heart health. Your heart will also be checked regularly during the treatment when starting different therapies and after you are done with treatment. These are some standard tests used to check your heart:
A physical exam is a review of your body for signs of disease. Your doctor may listen to your heart with a stethoscope during this exam. If it does not sound normal, there may be damage to your heart.
Chest X-ray is a type of imaging test that takes pictures of the insides of your chest. Your doctor can see if your heart looks too big or fluid is building up in your lungs.
Echocardiogram is a type of imaging test that uses ultrasound. Ultrasound bounces sound waves off of organs to make pictures. Your doctor may use an echocardiogram to see your heart in action. Your doctor can see if your heart is pumping enough blood. This is the test used to measure LVEF.
ECG (electrocardiogram) is a test that measures the heart’s electrical activity. It lets your doctor see your heart rhythm in detail.
MUGA (multi-gated acquisition) scan is a test that injects a radiotracer into your vein. The radiotracer attaches to red blood cells. Next, a special camera is used to see the radiotracer through your heart. Your doctor can then see how well your heart is pumping. Your doctor can also see how well the blood vessels to the heart are working.
Troponins are proteins found in heart muscle. Troponins are released by dying heart cells and then enter the bloodstream. Troponin blood tests are done less often.
Troponins may be in your blood even before a decline in LVEF is seen. The use of troponins in the blood to predict heart problems is still being studied.
How can cardiac toxicity be prevented?
Cardiac toxicity can often be prevented by giving less of the cancer drug. Also, you could get lower doses more often instead of larger amounts less often. There may be less toxic drugs. For example, doxorubicin liposome injection, a liposomal anthracycline, is less toxic than regular doxorubicin.
The problem is balance. You don’t want more treatment than is needed to treat the disease. Then again, you don’t want to undertreat cancer to lower the chance of side effects. It would help to talk to your doctor about the balance of risks and benefits of cardiotoxic treatment.
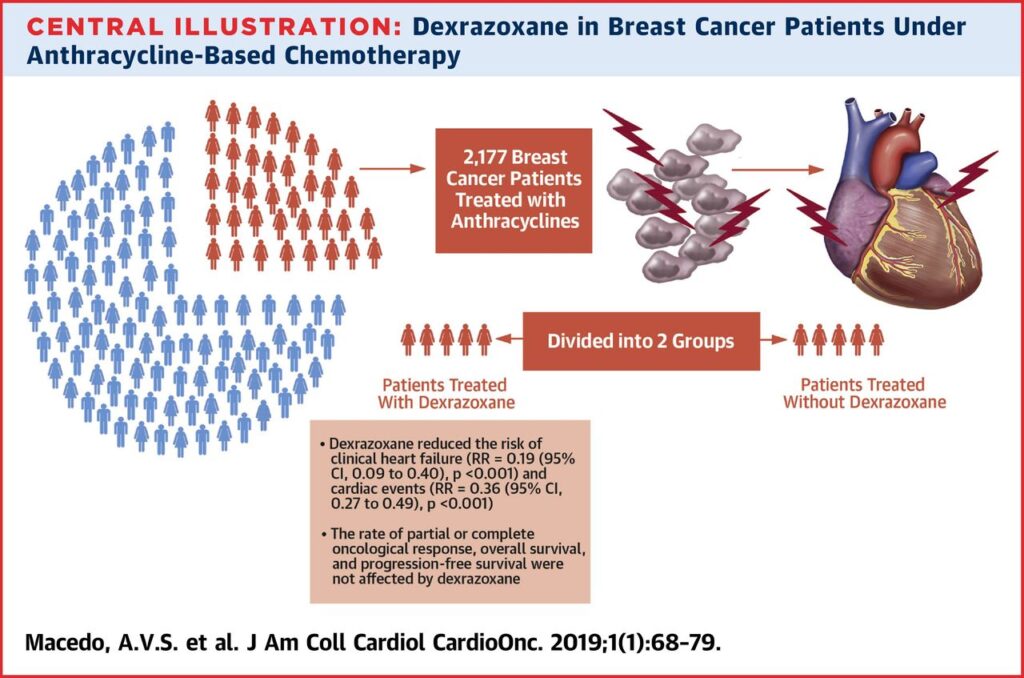
For breast cancer, sometimes dexrazoxane (Zinecard®) is used to prevent or lessen heart damage caused by doxorubicin or epirubicin. It is given right before either drug to protect your heart.
Other drugs are now being tested for the prevention of damage to the heart in high-risk patients. These include enalapril, an ACE (angiotensin-converting enzyme) inhibitor, and carvedilol, a beta-blocker.
How is cardiac toxicity treated?
If treatment for cardiac toxicity is started early, it is more likely that serious heart damage will be prevented. If you have heart failure because of cancer treatment, you will be treated like other patients with heart failure. You may be given some combination of these medicines:
A diuretic (to control your fluids),
An ACE inhibitor (to control your blood pressure),
A beta-blocker (to control your blood pressure), or
A digitalis drug (to make your heart stronger and to regulate heart rhythm).
In severe cases, a heart transplant may be needed.
